Sleep Disorder Consultation
Diagnosing Your Sleep Disorder
Central Florida Sleep Institute is committed to making a thorough assessment of your sleep issues so that we can fully understand your condition and create a treatment plan specific to your needs.
Using a multi-disciplinary approach, we not only look at the problems you’re experiencing with sleep, but the underlying causes –and effects– when diagnosing and treating your sleep issues. We also have a full range of tests at our disposal to help our physicians gain an understanding of your condition.
Procedures
Central Florida Sleep Institute has a full range of testing procedures and technology at its disposal to help diagnose your sleep disorder. Some of the tests require a visit to the clinic, while others can be done at home.
Learn more about the various methods the Sleep Clinic may employ to assess
- your sleep
- Consultation
- Overnight sleep study
- Daytime sleep study
- Home sleep study
Consultation with Sleep Specialist
Central Florida Sleep Institute faculty is extremely knowledgeable about all types of sleep disorders. The clinic has specialty clinics specifically tailored for patients with insomnia, narcolepsy and restless legs syndrome. No matter what your reason for visiting the Sleep Clinic, you can be sure that our physicians will do everything they can to help.
During a consultation appointment, your doctor will do a short physical exam and discuss the information you provided in a questionnaire completed before your appointment. Based on your symptoms and history, you and your doctor will develop a treatment plan to resolve your sleep complaints.
Overnight, Attended Sleep Study
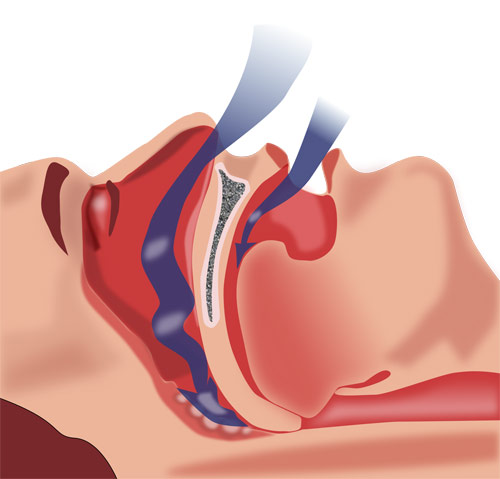
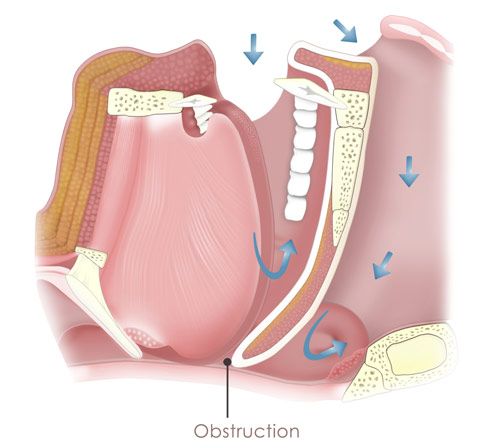
Overnight, attended sleep studies – known as nocturnal polysomnograms (PSG)– are conducted in a sleep lab where you’re monitored (or attended) all night by a trained sleep technologist. Your doctor may recommend a sleep study to diagnose or rule out a sleep disorder such as obstructive sleep apnea, narcolepsy or periodic limb movement disorder. You may also undergo a sleep study if you’ve already been diagnosed with a sleep disorder so that we can create or adjust your treatment plan.
During the study, we assess your sleep stages by recording brainwaves (EEG), eye movements (EOG) and muscle tone (EMG). We also carefully examine your breathing throughout the night by measuring your airflow, breathing effort, snoring and oxygen saturation. Leg movements and heart rate (ECG) are also monitored to provide a comprehensive evaluation of your sleep. Collecting all this data requires the sleep technologist to apply numerous sensors before you go to sleep. The set up procedure is quite complex and usually takes about 90 minutes. The hook up includes applying sensors on the scalp, face, throat, chest, finger and legs.
There are three common types of overnight sleep studies:
Diagnostic Evaluation:This study measures your sleep without any intervention. It’s typically used to diagnose or rule out a disorder.
Continuous Positive Airway Pressure (CPAP) Titration: During a CPAP titration, the technologist adjusts the setting on the CPAP machine to determine how much air pressure is needed to normalize your breathing.
Split Night Study: A split night study is a combination of a diagnostic and CPAP titration study. The first half is used to diagnose sleep apnea and then midway through the night CPAP is started. The sleep tech spends the rest of the night adjusting the pressure until breathing has been normalized.
Daytime, Attended Sleep Study
It can be very helpful to monitor a person during the day because it allows us to gain more insight about their daytime sleepiness. A daytime study is almost always preceded by an overnight sleep study. The daytime study uses many of the same sensors on the scalp and face we use for a nighttime study but does not usually include the sensors used to monitor breathing.
There are two different tests we conduct during the day:
Multiple sleep latency test (MSLT):
This test is the most common way to objectively quantify sleepiness and is a key test in diagnosing narcolepsy. The MSLT is comprised of 4-5 trials or “naps” spaced throughout the day. During the test, you’re asked to relax and try to fall asleep. There are two key pieces of information we gather from this study –the mean sleep latency, which is the average time it took you to fall asleep for all your naps, and the number of REM periods. Whether or not REM sleep was identified is evaluated since it’s atypical for a normal sleeper to have REM sleep during such a brief sleep period. Documenting REM in two or more of the trials can be a positive indication of narcolepsy used in combination with a clinical history.
Maintenance of wakefulness test (MWT):
The MWT is also a series of trials throughout the day, but instead of measuring your ability to fall asleep, it measures your ability to stay awake for a defined period of time under sleep-inducing circumstances. The test is based on the idea that, in some cases, your ability to stay awake may be more important than your ability to fall asleep. The MWT may be better suited for extremely tired individuals because it’s not confined by the floor effect that limits the MSLT. This test is commonly used to document the effective treatment of a sleep disorder for the Department of Motor Vehicles or for an employer.
Home Sleep Study to test for OSA
A home sleep study is a simplified version of an overnight, attended sleep study that focuses on nocturnal breathing. Home sleep studies are only used to diagnose or rule out obstructive sleep apnea (OSA). Because the emphasis is on breathing, it’s possible to use fewer sensors.
Not all patients are good candidates for a home test and not all insurance carriers will cover the cost of the study. If you need a sleep study, your doctor will make a recommendation based on your specific situation whether you should have your test done in the lab or at home.
Home Sleep Portable Monitoring:
If you’ve been scheduled for a home sleep study, you’ll need to pick up the equipment from the Sleep Institute. You’ll meet with a sleep technologist to learn how to properly place the sensors and start the study. That night, before bed, you’ll need to secure sensors to your upper lip, throat, chest, abdomen and finger. These sensors will record information about your airflow, snoring, breathing effort, heart rate and oxygen levels throughout the night. In the morning, you’ll remove the sensors, return everything to the test kit and return the equipment to the Sleep Institute so we can download and analyze the data.
Actigraphy:
Actigraphy is a non-invasive technique used to assess cycles of activity and rest over several days to several weeks. Your doctor may ask you to wear an actigraph for a period of time to get an objective measurement of your sleep schedule. An actigraph is worn like a watch on the wrist of your non-dominant hand and measures activity through light and movement. Actigraphy data can be very helpful for assessing circadian rhythm disorders such as advanced or delayed sleep phase disorder and insomnia.
Sleep Diary
Your physicians may ask you to fill out a sleep diary or sleep log each day to document specific sleep and wake habits over a period of time. A sleep diary can be particularly useful in diagnosing and treating insomnia and circadian rhythm disorders. A sleep diary can be a very helpful tool to gain more insight into your sleep problem, or to monitor whether a treatment is successful. Sleep diaries are normally completed once or twice a day. It usually consists of several questions related to sleep and wake times, nap times, caffeine and alcohol use and general mood or functioning.
